HIV Pathogenesis Research
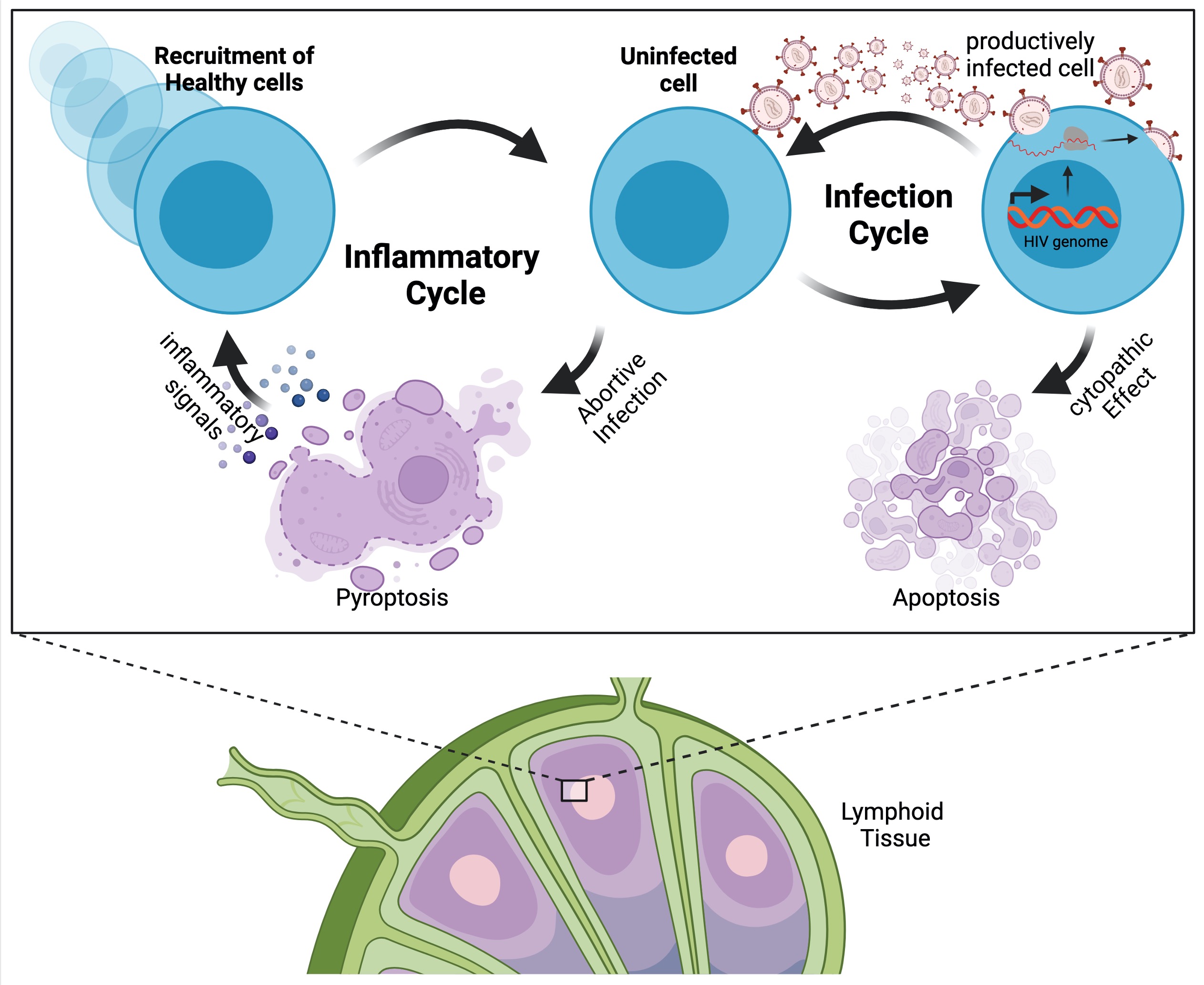
HIV pathogenesis is primarily driven by incomplete infections, where the virus is intracellularly recognized and successfully combated by tissue-resident immune cells. However, such an "abortive infection" leads to a pro-inflammatory cell death (pyroptosis) of the affected cell, which in turn contributes to the migration of new, HIV-susceptible cells. Since these cells are often also incompletely infected, an inflammatory cycle ensues, causing more and more immune cell death, ultimately leading to AIDS.
We strive to explore the modulation of pyroptotic cell death in HIV infections by different extrinsic and host factors. We believe that the cellular context strongly influences infection outcomes, abortive infections and therefore HIV-induced cell death. A better understand of these factors could have important implications for the development of better (personalized) therapeutic strategies or novel diagnostic tools.
HIV-induced pyroptotic cell death can be studied exclusively in tissue-derived CD4 T cells. Our research is therefore based on CD4 T cells from tonsils provided by the Clinic for Head and Neck Surgery of the University Hospital Essen. We use different flow cytometry and plate reader assays to probe pyroptosis upon in vitro HIV infection of tissue-resident CD4 T cells. In addition we also seek to establish cell line models of pyrptosis in order to facilitate high-troughput testing of potential anti-inflammatory treatments.

